Circumcision - Urinary Tract Infections
For a systematic review and meta-analysis in the Journal of Urology see: [Morris & Wiswell, 2013]. This study found that the single risk factor of lack of circumcision confers a 23% chance of urinary tract infection (UTI) over the lifetime. Over their lifetime 32% of uncircumcised males experience a UTI, as compared with only 8.8% of circumcised males. Highest risk is in infancy, where UTI is 10-times higher in uncircumcised males.
Infections of the urinary tract are regarded as being COMMON in the pediatric population [Koyle et al., 2003] and can lead to significant morbidity [Chon et al., 2001]. The highest prevalence and greatest severity of UTIs in boys is prior to 6 months of age [Wiswell, 1997a; Schoen et al., 2000a], decreasing after infancy [Zorc et al., 2005a]. The younger the infant, the more likely and severe will be the UTI and the greater the risk of sepsis and death [Schoen, 2005c]. In western Sydney, by the age of 7 years, 2% (definitely) and another 5% (probably) of boys have had at least one UTI [Sureshkumar et al., 2009].
UTI in children can involve just the lower urinary tract (acute cystitis) and/or infection of the kidney itself (acute pyelonephritis) [Bensman & Ulinski, 2009].
A preliminary study in Sweden has shown that early breastfeeding might also lower UTI [Marild et al., 2004], but, whilst worthwhile for many reasons, is less effective, and cannot be advocated as a replacement for circumcision. Moreover, a New Zealand study found no relationship between circumcision status and breastfeeding outcomes, nor health and cognitive ability outcomes [Fergusson et al., 2007]. Thus circumcision does not disrupt breastfeeding. In fact in this study uncircumcised infants had twice as many lower respiratory tract infections (21% vs. 11%) [Fergusson et al., 2007]. Research showing an association of UTI with lack of circumcision is extensive and the link is now unequivocal. Most of the evidence has emerged over the past 25 years or so.
High risk of UTI conferred by lack of circumcision:
INFANTS AND CHILDREN:
In 1982 it was reported that 95% of UTIs in boys aged 5 days to 8 months were in uncircumcised infants [Ginsburg & McCracken, 1982]. This was confirmed by Wiswell in 1982 and a few years later Wiswell and colleagues found that in 5261 infants born at one US Army hospital, 4% of UTI cases were in uncircumcised males, but was only 0.2% in those who were circumcised [Wiswell et al., 1985]. This relatively captive population in Hawaii was said to be more reliable than the rate reported for hospital admissions [Wiswell, 2000].
Wiswell then went on to examine the records for 427,698 infants (219,755 boys) born in US Armed Forces hospitals from 1975-79 and found that the uncircumcised had an 11-fold higher incidence of UTIs [Wiswell & Geschke, 1989]. During this decade the frequency of circumcision in the USA decreased from 84% to 74% and this decrease was associated with an increase in rate of UTI [Wiswell et al., 1987]. Reviews by others in the mid-80s concluded there was a lower incidence in circumcised boys [Roberts, 1986; Lohr, 1989].
The rate in girls was stable during the period it was increasing in boys, in whom circumcision was in a decline. In a 1993 study by Wiswell of 209,399 infants born between 1985 and 1990 in US Army hospitals worldwide, 1046 (496 boys) got UTI in their first year of life [Wiswell & Hachey, 1993]. The number was equal for boys and girls, but was 10 times higher for uncircumcised boys. Among the uncircumcised boys younger than 3 months, 23% had bacteremia, caused by the same organism responsible for the UTI.
In a study of 14,893 male infants aged less than 1 year who had been delivered during 1996 at Kaiser Permanente hospitals in Northern California, with 65% circumcised, 86% of the UTIs occurred in the uncircumcised boys [Schoen et al., 2000a; Schoen et al., 2000c]. The mean cost of management in the boys was US$1,111, being twice that of girls (US$542), reflecting a higher rate of hospital admission in uncircumcised males with UTI (27%) compared with females (7.5%). Mean age at admission also differed: 2.5 months for uncircumcised boys vs 6.5 months for girls. Total cost was 10-times higher for uncircumcised boys vs girls ($155,628 vs $15,466).
There were 132 episodes of UTI in uncircumcised males, but only 22 in those who had been circumcised. Hospital admissions were 38 vs 4, respectively. Incidence during the first year of life was 2.2% in uncircumcised boys and just 0.22% in circumcised boys (odds ratio = 9:1). The incidence in the girls was 2%. In a commentary to this article, Wiswell points out that half of infants with acute pyelonephritis get renal scarring that then goes on to predispose to serious, life-threatening conditions later in life, meaning also a large, ongoing cost [Wiswell, 2000]. If circumcisions were no longer done in the USA one woud expect 20,000 cases of acute pyelonephritis annually [Roberts, 1996]. Unlike adults, children, especially the very young, are more likely to develop such renal injury and scarring. In fact imaging studies have shown that 50-86% of children with febrile UTI and presumed pyelonephritis have renal parenchymal defects [Rushton & Majd, 1992b], which persist. Nuclear scans following the treatment of UTI in febrile infants have noted scarring in 10-30% of cases [Hoberman et al., 1999]. In a 27-year follow-up study risk of hypertension in these was 10-20%, and 10% were at risk of end-stage renal disease [Jacobson et al., 1989].
The UTI may be accompanied by increased sodium excretion, decreased filtration by the kidney and high levels of the pressor agents renin and aldosterone [Schoen et al., 2002]. In febrile infants bacteruria is seen in 36% of uncircumcised boys, indicating that a UTI is the likely cause of the febrile symptoms, but was only 1.6% of those who were circumcised, a 22.5-fold difference [Hsiao et al., 2006].
UTIs are thus far from benign disorders of infancy. Moreover, the AAP Subcommittee on Urinary Tract Infections recommends a urine culture for any child under 2 with unexplained fever.
It should be noted that these studies gave figures for infants admitted to hospital for UTI, so that the actual rate would undoubtedly have been higher. Moreover, many fevers for which infants are admitted could have an undiagnosed UTI as the basis. The rate of UTI in uncircumcised boys may thus be higher than 2%.
The infection can travel up the urinary tract to affect the kidney, so explaining the higher rate of problems such as pyelonephritis referred to above and renal scarring (seen in 7.5% [Ramet et al., 1997]) of uncircumcised children [Stull & LiPuma, 1991; Rushton & Majd, 1992a]. In those with febrile UTI, 34%-70% have pyelonephritis [Zorc et al., 2005a]. And, as mentioned above, imaging studies have revealed renal parenchymal defects in 50-86% of children with febrile UTI and presumed pyelonephritis [Rushton & Majd, 1992b]. In the first year of life 90% of UTIs have pyelonephritis [Rushton, 1997b]. Of those with acute pyelonephritis, 36-52% will subsequently develop renal scarring [Rushton, 1997b], [Wallin & Bajc, 1993; Jakobsson et al., 1994; Benador et al., 1997].
The E. coli responsible for UTI form impenetrable, protective “pods” on the walls of the bladder, so explaining the well-known ability of the bacteria responsible for UTI to persist in the face of robust host defences and antibiotic administration [Anderson et al., 2003; Mysorekar & Hultgren, 2006]. Such a mechanism explains recurrent UTIs.
Alarmingly, amongst boys with UTI, 19% of those uncircumcised experienced recurrent UTIs, whereas none of the circumcised did [Conway et al., 2007].
Premature uncircumcised boys had an 11-fold increase in risk of UTI and circumcision eliminated the risk of recurrence of UTI in a study in Augusta, Georgia [Cason et al., 2000].
These and other reports – e.g., [Ginsburg & McCracken, 1982; Glennon et al., 1988; Herzog, 1989; Crain & Gershel, 1990; Stull & LiPuma, 1991; Rushton & Majd, 1992b; Rushton & Majd, 1992a; Spach et al., 1992; Craig et al., 1996; Shaw et al., 1998; Cason et al., 2000; World, 2008b] – all point to the benefits of circumcision in reducing UTI. Because UTIs are associated with long-term morbidity and potential mortality [Koyle et al., 2003], prevention by measures such as infant male circumcision is highly desirable.
Wiswell performed a meta-analysis of all 9 studies that had been published up until 1992 and found that every one had observed an increase in UTI in the uncircumcised [Wiswell & Hachey, 1993]. The average was 12-fold higher and the range was 5- to 89-fold, with 95% confidence intervals of 11-14 [Wiswell & Hachey, 1993]. Meta-analyses by others have reached similar conclusions. A meta-analysis in 2005 of one (very small) randomized controlled trial [Nayir, 2001], 4 cohort studies, and 7 case-control studies found 8-fold higher UTI in uncircumcised boys (95% CI: 5-13) [Singh-Grewal et al., 2005]. This slightly lower estimate is from inclusion of data for older boys, and the conservative recommendations by the authors of this paper have been criticized [Schoen, 2005c]. This meta-analysis noted 1,222 UTIs in 107,873 uncircumcised infants, i.e., 1.1%, and the summary OR for the protective effect of circumcision against UTI was 0.13 (95% CI 0.08 - 0.20), i.e., circumcision reduced UTI 7.7-fold [Singh-Grewal et al., 2005]. In Sweden (where infant circumcision is rare), cumulative incidence of UTI was 2.2% by age 2 [Jakobsson et al., 1999]. A meta-analysis published in 2008 found that amongst febrile male infants aged less than 3 months (the age group with highest prevalence of UTI), UTI was the cause of the fever in 20.1% of uncircumcised boys, but only 2.4% of boys who were circumcised [Shaikh et al., 2008]. Prevalence was almost twice as high in white as in black boys. In febrile girls aged 0-3 months UTI prevalence was 7.5%. Among older children (< 19 years) pooled prevalence of UTI (both afebrile and febrile) was 7.8%.
A large study in Canada of equal numbers of neonatally circumcised and uncircumcised boys saw rates of UTI and hospital admissions for UTI that were 4-fold higher in the uncircumcised [To et al., 1998]. In Australia, a relatively small study in Sydney involving boys under 5 years of age (mean 6 months) found that 6% of uncircumcised boys got a UTI, compared with 1% of circumcised [Craig et al., 1996]. A US study of 1025 febrile infants aged less than 2 months found the cause was UTI in 21.3% of uncircumcised boys, 2.3% in circumcised boys, and 5% in girls [Zorc et al., 2005b]. Odds ratio of UTI associated with being uncircumcised was 10.4 (bias-corrected 95% CI: 4.7-31.4) in this study. In the Pediatric Research in Office Settings' Febrile Infant Study of 219 US practices, being uncircumcised was the strongest multivariate predictor of UTI, with an odds ratio of 11.6 (95% CI 5.9-22.6) [Newman et al., 2002]. Another US study found 10.3% of febrile infants aged 2-6 months had serious bacterial illness, the proportion being similar for girls and boys [Hsiao et al., 2006]. The incidence of serious bacterial illness was 36% in the uncircumcised and 1.2% in the circumcised, i.e., was 22.5 times higher in the uncircumcised.
A study of UTIs to age 16 in the UK noted a cumulative incidence of 3.6% [Coulthard et al., 1997].
According to a personal communication from Dr Tom Wiswell in 2005: “The best data indicate that ~2.5% of uncircumcised boys will have a UTI during the first year of life. The lowest percentage among studies is ~1.1%. There are approximately 130 million births around the world annually. A little more than half are boys. Of these 65 million boys, probably 80% or more are not circumcised (52 million). Thus, worldwide there would be anywhere from 560,000 to 1.45 million uncircumcised boys with UTIs annually. This does not include older uncircumcised males who are also more prone to have UTIs, but at much lower rates.”
Although UTIs are low in Jewish boys, who are all circumcised at day 8 after birth, those circumcised by a physician have a 2.8-fold lower incidence of UTI than those circumcised by a religious authority [Prais et al., 2009].
UTI in Japanese boys aged 0-6 months were more likely to have a meatus that was covered tightly by the foreskin compared to healthy boys (85% vs 42%) [Hiraoka et al., 2002]. In this study, the foreskin covered the external urethral meatus in 96% of healthy boys aged less the 3, and a a gentle retraction procedure was unable to uncover the meatus in 40% of those aged 0.6 months. The recurrence rate of UTI in Korean boys aged 0-6 months was 26% compared with 7.7% in older infants [Shim et al., 2009]. Recurrent UTI was seen in 34% of those with nonretractile foreskins compared with 18% of those whose foreskin could be retracted [Shim et al., 2009]. Acute pyelonephritis increased the likelihood of recurrent UTI by 4.6 [Shim et al., 2009]. Nonretractile foreskin and acute pyelonephritis were the biggest risk factors for recurrent UTI. Acute pyelonephritis is a major cause of renal scarring [Elder, 2007b]. It occurs even in the absence of vesicoureteral reflux and in this study had an incidence of 36% [Shim et al., 2009]. Posterior urethral valves are the most common cause of end-stage renal failure in childhood. Circumcision reduces the incidence of UTIs in such boys (mean age 6.7 years, range 1-18) by 83-92%, with every circumcision preventing one UTI on average [Mukherjee et al., 2009]. Early circumcision of boys with posterior urethral valves was thus advocated.
Despite the strong evidence and enormous differential, a randomized controlled trial (RCT) would provide the gold standard seal of support to the protection afforded by circumcision against UTIs. The only previous RCT was of 70 boys of mean age 3.5 (range 3 months to 10 years) with normal renal ultrasonography who had microbiologically confirmed UTI [Nayir, 2001]. One group of 35 boys had monthly urine cultures over a 6-month period, and when positive (with or without any symptoms), they received antibiotic treatment. After 6 months they were circumcised and then observed for another 6-month period. The rate of positive urine cultures in these boys dropped from 3.6 ± 1.1 to 0.14 ± 0.35 episodes after circumcision (P<0.001), i.e., circumcision decreased UTI by 96%. Another group of 35 boys were circumcised immediately after the first UTI and were followed for 6 months. The rate of significant bacteriuria during the period after circumcision was 0.17 ± 0.38 episodes. A larger study is probably unnecessary, but could be considered. This might involve a cohort of parents who are equivocating about whether to have their newborn son circumcised, and the circumcised and uncircumcised boys could then be followed for a year. To ensure all are otherwise treated the same, suprapubic aspiration would be needed for sample collection for urinalysis in each case, even though uncontaminated urine can be obtained from circumcised boys when they urinate naturally. However, given the striking and consistently higher rate of UTIs in uncircumcised boys in all studies to date, it might be difficult to obtain ethical approval for a study like this in which the outcome is virtually guaranteed.
UTI IN ADULTHOOD:
The benefit appears to extend beyond childhood and into adult life. In a Seattle study of men aged, on average, 32 years, and matched for race, age and sexual activity, the circumcised had a 5.6-fold lower rate of UTI [Spach et al., 1992]. A lifetime prevalence of UTI in a large, nationally-representative US study of men aged 18-85+, was 13.7% [Griebling, 2005; Griebling, 2007]. This did not take into consideration circumcision status. Based on a circumcision rate of 79% in the USA [Xu et al., 2007] it can be estimated that up to 44% of uncircumcised men, compared with 6% of circumcised men will get a UTI over their lifetime (J.H. Waskett and B.J. Morris, unpublished results - see diagram below).
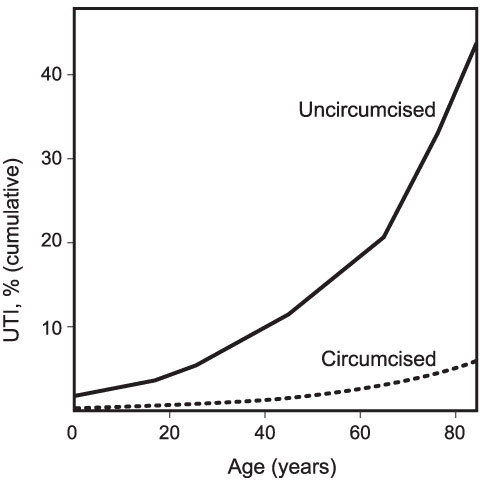
Very high cumulative prevalence of urinary tract infections in uncircumcised males over their lifetime (from calculations by J.H. Waskett; unpublished).
UTI is the most costly (over $1 billion in men [Griebling, 2005]) and resource intensive urological condition in the USA, with 1.8 million physician visits [Litwin et al., 2005]. Circumcision may reduce this burden.
A report in 2010 identified the entire microbiome of the penis of 12 men before and after circumcision [Price et al., 2010]. Among the 42 unique bacterial families identified, Pseudomonadaceae and Oxalobactericeae were the most abundant irrespective of circumcision status. Circumcision was associated with a significant change in the overall microbiota (P = 0.007) and with a significant decrease in putative anaerobic bacterial families (P = 0.014). Two families in particular - Clostridiales Family XI (P = 0.006) and Prevotellaceae (P = 0.006) - were uniquely abundant before circumcision. Within these families the authors identified a number of anaerobic genera previously associated with bacterial vaginosis including: Anaerococcus spp., Finegoldia spp., Peptoniphilus spp., and Prevotella spp. The researchers concluded that the anoxic microenvironment under the foreskin may support pro-inflammatory anaerobes that can activate Langerhans cells to present HIV to CD4 cells in draining lymph nodes. They suggested that the reduction in putative anaerobic bacteria after circumcision may play a role in protection from HIV and other sexually transmitted infections.
Bacteria:
The fact that fimbriated strains of the bacterium Escherichia coli which are pathogenic to the urinary tract and pyelonephritogenic, have been shown to be capable of adhering to the foreskin, satisfies one of the criteria for causality [Kallenius et al., 1981a; Kallenius et al., 1981b; Fussell et al., 1988; Glennon et al., 1988; Wiswell et al., 1988; Stull & LiPuma, 1991]. In a prospective study of 25 boys who underwent circumcision for medical reasons, specimens of periurethral bacterial flora were taken prior to as well as 3 weeks after surgery [Wijesinha et al., 1998]. Before circumcision, 52% harboured uropathogenic organisms (E. coli and other coliforms 93%, Enterococcus spp 9%, Proteus spp 8%, Pseudomonas spp 4%, and Klebsiella spp 2%), but after circumcision, none of the boys had uropathogens. It was postulated that circumcision converts a 'cul-de-sac' that is a reservoir of organisms capable of causing ascending UTI into a surface colonized by natural skin organisms. This study supports the idea that circumcision protects against UTI.
In another study, in 2004, pathogenic bacteria were reported to be present in the peri-urethral region of 64% of boys (without phimosis) prior to circumcision, but in only 10% four weeks after circumcision [Gunsar et al., 2004]. For the glanular sulcus these figures were 68% and 8%, respectively, and the bacteria were similar in each location. This study concluded that the origin of periurethral flora is the deeper preputial regions and also emphasized the beneficial role of circumcision [Gunsar et al., 2004].
A similar study in boys aged 4 to 12 (mean 6) found that the 16% with phimosis had clinically significant uropathogenic bacterial colonization (greater than 100,000 cfu/ml). In the rest (i.e., the 84% without phimosis) 56% had uropathogenic species in their foreskin and in 93% of these the levels were clinically significant. Harmless species were seen in 15%, and in 30% no bacterial growth was found [Tokgoz et al., 2005]. Frequency of species overall was: 3% E. coli, 19% Klebsiella, 13% Staphylococci, and 44% Enterococcus. Thus significant preputial colonization by uropathogens persists in preschool and primary school children.
Thus in infancy and childhood the prepuce becomes colonized with bacteria. Fimbriated strains of Proteus mirabilis, non-fimbriated Pseudomonas, as well as species of Klebsiella and Serratia also bind closely to the mucosal surface of the foreskin within the first few days of life [Wiswell et al., 1987; Fussell et al., 1988; Glennon et al., 1988]. Circumcision prevents such colonization and subsequent ascending infection of the urinary tract [Roberts, 1986].
Swabs taken of the periurethral area (the region of the penis where urine is discharged) in 46 circumcised and 125 uncircumcised healthy males (mean age = 27; range = 2 to 54 years) showed a predominance of Gram positive cocci in both groups, facultative Gram negative rods in 17% of uncircumcised males, but in only 4% of circumcised (P = 0.01) [Serour et al., 1997]. Streptococci, strict anaerobes (bacteria that can grow without oxygen) and genital mycoplasms (bacteria that lack a cell wall) were found almost exclusively in uncircumcised males over the age of 15 years (82% of the study group) [Serour et al., 1997].
Since these organisms are common inhabitants of the female genital tract, acquisition via sexual transmission was suggested. These latter categories of bacteria, unlike the Gram positive cocci, are potential pathogens capable of causing UTIs. It was speculated that when Gram negative organisms are the only colonizers of the preputial space they achieve higher concentrations and that the quantitative difference may contribute to the development of UTI. The findings of this study provide a microbiological basis for the observed higher risk of UTI in uncircumcised adult men. The authors also concluded that their results pointed to a role for the prepuce as a reservoir for sexually transmitted organisms [Serour et al., 1997].
Another study, conducted in Dublin, involving swabs from the periurethral area, found that antibiotic prophylaxis in boys with vesicoureteral reflux was not effective in reducing the bacterial colonization of the prepuce, and recommended circumcision to reduce UTIs [Cascio et al., 2001]. Vesicoureteral reflux (VUR) increases risk of UTI, putting those boys in great danger from renal damage [Fischbacher, 1999]. But it is the parenchymal infection and inflammation, rather than the VUR, that is the prerequisite for renal scarring [Wallin & Bajc, 1993; Benador et al., 1997; Rushton, 1997a]. Moreover, the majority of children with renal scarring do not have VUR [Rushton, 1997a].
Circumcision, as an adjunct to prophylactic antibiotics, is advocated for all boys with severe uropathy whose main clinical problem is recurrent UTI [Thiruchelvam & Cuckow, 2005]. Salmonella typhimurium has also been found (in a 10 month old boy) and circumcision not only prevented further UTI, but also the spread of this organism to the general public [Sonmez et al., 2001].
A randomized controlled trial of children of average age 14 months (64% girls and 42% with a history of VUR) found a small but significant reduction in symptomatic UTI in those given long-term antibiotic treatment (UTI arose in 13% of antibiotic group versus 19% of placebo group during the 12 month study period) for recurrent UTI [[Craig et al., 2009]. For those with fever as well the difference was stronger (7% versus 13%). It was suggested that such therapy for infants at high risk of infection was warranted, but should not be recommended routinely for those with a single symptomatic UTI.
Whereas 92% of boys aged 0–6 tested positive for bacteria under the foreskin, this diminished to 73% for boys aged 6–12, and was accompanied by a shift from enteric pathogens to normal skin flora [Agartan et al., 2005].
An absence of CD8 T lymphocytes in the foreskin may help the colonization of uropathogenic bacteria [Balat et al., 2008]. In this study Langerhans cells were much higher in foreskin than normal skin.
Yeast fungi:
In boys (mean age 5.8 years, range 0.01-13) colonization of the glans penis by yeast was 11.7% just prior to circumcision and 1.3% one month later [Aridogan et al., 2009]. The species found were Candida albicans (50%), Malasserzia furfur (40%) and Malassezia sympodialis (10%).
Consequences:
Since the absolute risk of UTI in uncircumcised boys is approx. 1 in 25 (0.05) and in circumcised boys is 1 in 500 (0.002), the absolute risk reduction is 0.048. Thus 20 to 50 baby boys need to be circumcised to prevent one UTI. However, the potential seriousness and pain of UTI, which can in rare cases even lead to death, should weigh heavily on the minds of parents.
Obtaining a midstream urine sample for culture from a circumcised boy is easy [Bailis, 1997]. However, valid urine samples from uncircumcised boys requires invasive techniques such as transurethral catheterization or suprapubic bladder aspiration [Bailis, 1997; American., 1999; Koyle et al., 2003; Cheng & Wong, 2005; Schroeder et al., 2005]. Only a urinalysis can distinguish UTI as a cause of fever as distinct from upper respiratory tract or ear infection (otitis media), it being noted that "one would be amazed at the number of children with renal scarring who have had treatment in the past for multiple episodes of 'otitis media' without urine cultures having been obtained" [Belman, 1997]. Indeed, the AAP recommends a urine culture for any child under 2 with unexplained fever assessed as being sufficiently ill to warrant antibiotic therapy [American, 1999]. The higher the fever and the longer its duration, the greater the likelihood of UTI [Roberts, 2002].
The complications of UTI that can lead to death are: kidney failure, meningitis and infection of bone marrow. In the first month of life 21-36% of infants with UTI have bacteremia, with concomitant meningitis being seen in 3-5% of these [Wiswell & Geschke, 1989; Bachur & Caputo, 1995]. Other acute complications of infant UTI are severe dehydration, electrolyte imbalances, transient pseudohypoaldosteronism, and cachexia [Wiswell & Geschke, 1989], with the youngest at risk of renal failure [Wiswell & Geschke, 1989; Bachur & Caputo, 1995] or death [Littlewood, 1972; Wiswell & Geschke, 1989]. The later consequences of renal scarring include hypertension (high blood pressure), hyposthenuria (urine with low specific gravity due to impaired concentrating ability of the kidney), and chronic renal insufficiency.
The latter may proceed to end-stage renal disease, which, like hypertension, is not seen by pediatricians because such conditions generally manifest in adulthood. Consequently pediatricians are not aware of the high health risk posed by a UTI. Of children with VUR and UTI followed to age 18, 1.5% died (renal failure being a cause), 1.5% had renal transplants, 3% borderline hypertension, 4% high serum creatinine (indicating impaired filtration by the kidney), and 8% were being treated for hypertension [Smellie, 1991]. Over 27 years of observation, 23% developed hypertension and all had reduced glomerular filtration rate as well as lower renal plasma flow, with 10% getting end-stage renal disease [Jacobson et al., 1992].
Costs for treatment are 17 times higher, based on 1-year cumulative incidence in circumcised and uncircumcised boys of 0.22% vs 2.15%, respectively, and cost in each was stated as $703 vs $1,179 in a report in 2000 [Schoen et al., 2000a]. These estimates did not include longer-term expenses such as tests for renal scarring, screening for subsequent infection and costs of morbid consequences of renal scarring. So actual cost from lack of circumcision is very much higher. Other estimates at the time put the cost of treatment of UTI by intravenous antibiotics for 3 days followed by oral for 11 days at $3577 as compared with $1473 for oral antibiotic for 14 days [Hoberman et al., 1999]. The efficacy of low-dose long-term antibiotics for children prone to develop recurrent acute pyelonephritis (VUR, obstructive nephropathies, etc) has been questioned as it does not reduce risk and can increase risk of resistant infections [Conway et al., 2007]. In contrast to antibiotic treatment, the efficacy of circumcision in reducing UTI is questioned far less [Bensman & Ulinski, 2009].
The data thus show that much suffering has resulted from leaving the foreskin intact. Lifelong genital hygiene in an attempt to reduce such infections is also part of the price that would have to be paid if the foreskin were to be retained. However, given the difficulty in keeping bacteria at bay in this part of the body [Oster, 1968; Schoen, 1993], not performing circumcision would appear to be far less effective than having it done in the first instance [Rushton & Majd, 1992a].
Moreover, the effectiveness of newborn circumcision in preventing UTI (> 90%) means it has a similar protective effect as many vaccines given to children to prevent diseases [Schoen et al., 2000c]. Thus, just as for immunization, in the era of preventative medicine circumcision should be promoted vigorously in an effort to prevent the hundreds of thousands of boys that are afflicted with this painful condition that can also have lifelong cardio-renal health implications, as well as fatal consequences.



